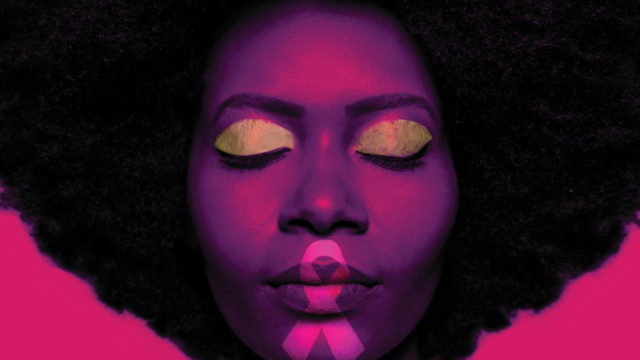
For women in the U.S., breast cancer is the most commonly diagnosed cancer and the second leading cause of cancer deaths.
According to the American Cancer Society (ACS), Black women have the highest death rate from breast cancer. Researchers partially attribute this to the fact that about one in five Black women with breast cancer have triple-negative breast cancer, which is more than any other racial or ethnic group.
Triple-negative breast cancer is a type of cancer in which cancer cells do not have the hormones estrogen or progesterone, or a protein called human epidermal growth factor (HER2). The absence of these specific receptors make it difficult for doctors to treat triple-negative breast cancer.
A mammogram is considered to be one of the best forms of screening for breast cancer and can help find breast cancer early, according to the U.S. Centers for Disease Control and Prevention (CDC). A mammogram is an X-ray of the breast. In 2016, the U.S. Preventive Services Task Force (USPSTF) recommended that women get screened every two years beginning at age 50 until 74.
However, a recent study published in the Journal of the American Medical Association (JAMA) suggested that Black women should start screening for breast cancer at an earlier age of 42, compared to white women who could start at age 57; American Indian/Alaska Native and Hispanic women at age 57; and Asian/Pacific Islander women at age 61. The study examined a total 415,277 breast cancer deaths in female patients of any age in the U.S. from 2011 to 2020.
According to the study, Black women have a 40% higher death rate than white women although Black women have an “incidence rate equal to the mean U.S. rate.” One finding that surprised Dr. Mahdi Fallah, one of three authors of the study and group leader of the Risk Adapted Cancer Prevention Group in the German Cancer Research Center, was the large difference in ethnicity and race-adapted starting age of breast cancer screening — up to 19 years difference between Black women (high risk) and Asian women (low risk).
“Cancer prevention should be personalized, meaning that preventive measures should be tailored to an individual’s risk profile,” Dr. Mahdi Fallah said in an email.
“To date, breast cancer screening guidelines have taken into account only a few factors, such as age and family history, ignoring some other readily available important factors such as ethnicity and race.”
Dr. Fallah noted that breast cancer clinical trials lack racial and ethnic diversity, with Black and Hispanic populations underrepresented. He explained that breast cancer mortality, pathological features and clinical outcomes vary among racial and ethnic populations, suggesting that an approach that considers race and ethnicity could “potentially” address existing disparities.
Personalized Breast Cancer Screening Urged for Black Women
“I think the article was interesting. One thing we do think over time, is that our goal [for]t screening becomes much more personalized and adaptable over time,” said Chief Scientific Officer Dr. William Dahut of the American Cancer Society. “So, screening for folks at average risk, I think, is a good starting place, but probably not nearly as helpful as if we can make screening much more personalized.”
Dr. Dahut referenced the changes in incidence and outcomes between Black and white women over the decades, and how those changes vary greatly across age and location now. Prior to the 1980s, the breast cancer mortality rate was slightly lower for Black women compared to white women.
Data from the CDC’s 2019 National Vital Statistics System reported that Washington D.C. (24.5), Nevada (23.7) and Nebraska (22.4) had the highest category for breast cancer death rates when adjusting for age. According to American Cancer Society 2023 data, California has the highest estimated new cases (32,020) than any other state so far.
Dr. Dahut explained that with varying death rates across states, it may be a matter of unequal access to timely and outstanding care, or “underlying biology.” As the study suggests that Black women be screened earlier, Dr. Dahut agrees that any evidence that supports Black women being screened earlier and often should be encouraged.
“The evidence-based results of our latest study urge health policymakers and clinicians to reconsider current screening guidelines. This is to ensure that screening is timely and appropriate for populations according to their risk profile,” Dr. Fallah shared in an email. “Other important steps include targeted public outreach and education initiatives to raise awareness and promote early screening among vulnerable groups.”
The USPSTF is currently working on updating its recommendation regarding mammograms for breast cancer screening. After examining models and small simulations to determine the best strategies for screening, the report found the models that used biennial screening beginning at ages 40 or 45 and ended at age 79 had the best outcome with mortality reduction compared to other strategies.
Authors of the study acknowledged the limitations of their work, including that higher mortality rates in Black women could be associated with inequitable access to breast cancer screening and treatment. The authors also noted that cancers that occur in young female patients are “inherently aggressive” regardless of race and ethnicity.
What women need to know about breast density and cancer risk
While several cancer research organizations and health organizations have varying standards on when women should be screened for breast cancer, the American College of Radiology (ACR) recommends all women begin screening beginning at the age of 40.
As a woman’s imaging expert and radiologist at Loma Linda University Medical Center, Dr. Cherie Cora follows recommendations set by the ACR. Dr. Cora has seen breast cancer occur earlier in Black women.
“I think it’s a decent article. I just think that everyone should be getting mammograms starting at age 40 anyway, just based on the ACR recommendations,” she stated.
In the last month, Dr. Cora has had three patients in their mid-30s come in, who had not gotten mammograms, who were diagnosed with cancer.
Dr. Cora said it’s hard to refer to previous literature regarding what data says about screening or the risk versus benefit of early screening when she sees people crying in front of her.
“I do understand that there’s anxiety that comes with screening, false positives and other things. But again, I have to look into the eyes of people who get diagnosed under age 40,” she explained. “I am sure I am somewhat biased in that I interact with these patients. I think that it’s worth it to that person to have found their cancer early.”
When a patient first begins screening for breast cancer, it is not uncommon to receive a call back from a doctor or radiologist because there is no foundation for breast imaging, so it takes time to get images or perhaps do additional testing to get a solid set of images.
Dr. Cora also recommends that patients be aware of different risk factors in the family such as relatives with breast cancer, genetic mutations in the family and breast density. Breast density refers to how much fibrous tissue and glandular tissue are in the breast compared to fatty tissue.
According to the CDC, women with dense breasts have a higher chance of being diagnosed with breast cancer, but breast cancer patients with dense breasts are not more likely to die from breast cancer than patients with less dense breasts. On a mammogram, fibrous and glandular tissue look white on a mammogram, and so does a potential tumor.
“The more white the background of your breast is, the harder it is to see through it, as opposed to someone who has much less dense breasts, and they have more fat, and fat is black,” Dr. Cora explained. “Now you’re looking for something white on a black background. It’s kind of like looking for the stars in the sky.”
California’s Breast Density Law, which was first enacted in 2013 and renewed by former Sen. Holly J. Mitchell in 2018, requires that women who have mammograms be informed if they have dense breast tissue by their doctors.









You must be logged in to post a comment Login